The most damaging moment in a medical facility isn’t always a surgical error or a misdiagnosis. Sometimes, it is simply the room going dark.
Consider a standard 10×10 exam room. A patient sits on the table, perhaps in a gown, feeling vulnerable. The physician is in the corner, typing notes into the Electronic Health Record (EHR) or listening to heart sounds. These are moments of stillness. Because commercial energy codes are written for bustling open offices or warehouses, the standard “energy-saving” sensor mounted in the corner decides the room is empty. The lights cut out.
The patient panics. The provider fumes. You will see doctors waving their arms over their heads like they are flagging down a rescue plane just to get the lights back on. This is the “waving arms syndrome.” It isn’t just a nuisance; it is a failure of care. When we design for healthcare, we aren’t just managing kilowatt-hours. We are managing trust. If the building fights the doctor, the patient loses confidence in the facility.
The Physics of Invisibility
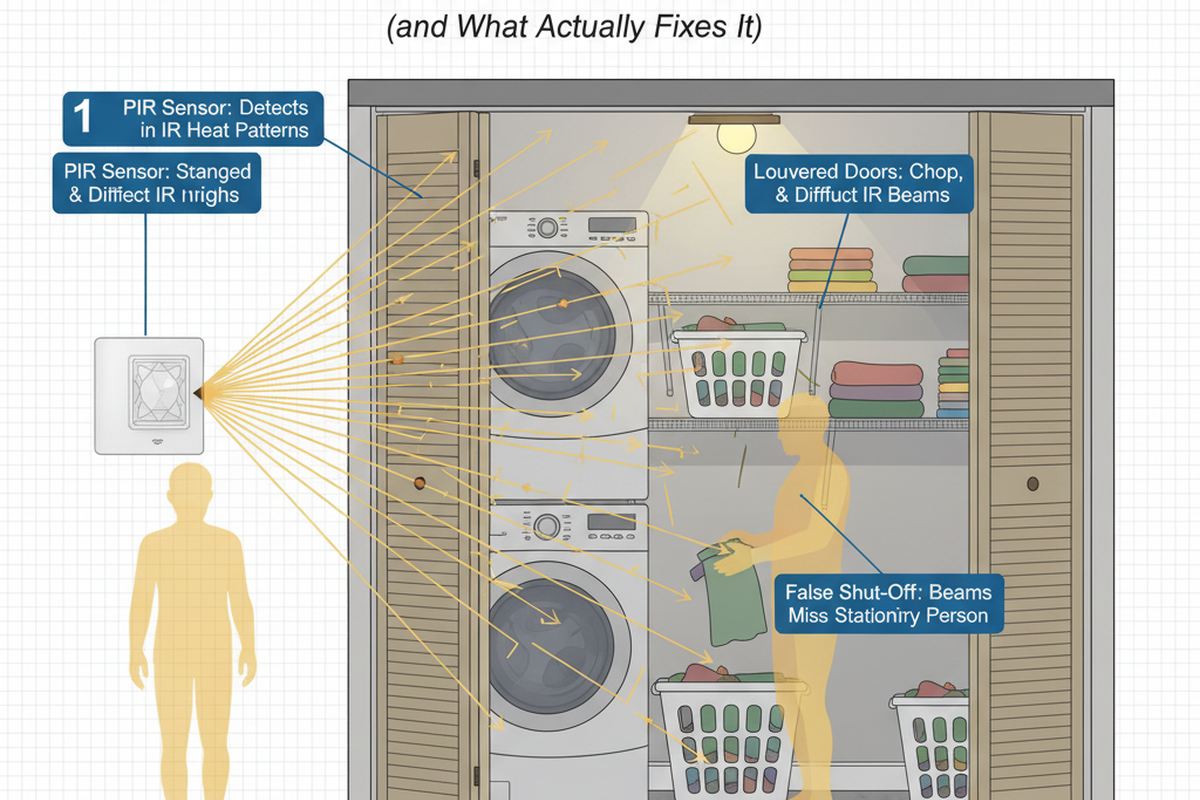
To fix this, we have to stop treating exam rooms like janitor closets. The root of the problem is the sensor technology itself. The vast majority of commercial sensors installed today are Passive Infrared (PIR).
PIR sensors work by detecting the movement of heat signatures across a field of view. They are excellent at detecting a person walking through a doorway or a forklift moving down an aisle—what we call “major motion.” However, they are fundamentally blind to “minor motion.” A doctor typing involves finger movement, but the heat differential is negligible from ten feet away. A patient sitting still while waiting for a consult is effectively invisible to a PIR sensor.
Room geometry makes it worse. In a gynecological or dermatology exam, privacy curtains are frequently drawn. A PIR sensor relies on line of sight. If a curtain blocks the sensor’s view of the physician, the sensor assumes the room is empty. I have seen retrofits where a PIR sensor was placed by the door; the moment the doctor stepped behind the curtain to begin a procedure, the timer started ticking down to a blackout.

The only viable solution for the patient zone is Dual-Technology (Dual-Tech). These sensors combine standard PIR with Ultrasonic detection. While PIR looks for heat in motion, Ultrasonic sensors fill the volume of the room with high-frequency sound waves (usually 32kHz or 40kHz) and listen for the Doppler shift caused by movement.
Ultrasonic sensors do not need line of sight. They can “hear” around the privacy curtain. They can detect the expansion of a chest cavity during breathing or the subtle shift of a person adjusting their posture on the exam table. Yes, they cost more than basic PIR units. Yes, they can occasionally be tricked by high-velocity HVAC airflow vibrating a poster on the wall. But in a clinical environment, a “false on” (wasting 15 minutes of LED energy) is infinitely preferable to a “false off” (scaring a patient).
Privacy and the “Manual On” Imperative
Once you have the right sensor, you have to program the logic correctly. This is where most electrical contractors, used to office buildings, get it wrong. They default to “Occupancy Mode” (Auto-ON/Auto-OFF).
In an exam room, Auto-ON is a privacy violation. Imagine a patient is half-dressed, waiting for the doctor. The door is cracked slightly for airflow or to signal the nurse. In a busy corridor, staff are constantly walking past that door. If the sensor is set to Auto-ON, every time a nurse walks by the gap, the lights in the exam room blast on to full brightness. It feels like an interrogation. It signals to the patient that they are exposed.
Maybe You Are Interested In
The only ethical configuration for an exam room is “Vacancy Mode” (Manual-ON/Auto-OFF). The lights should only come on when a human being intentionally hits the switch upon entering. This ensures the room remains dark or dim until the occupant is ready for light.
This setup also solves the “cleaning crew” dilemma facility managers often worry about. I often hear concerns that if we don’t use Auto-ON, the cleaners will leave lights on all night. But Vacancy Mode actually supports the cleaning workflow better: cleaners only turn on lights in the specific rooms they are scrubbing. If they skip a room, it stays dark. The Auto-OFF function remains as the safety net, catching any lights left on after the crew departs.
Looking For Motion-Activated Energy-Saving Solutions?
Contact us for complete PIR motion sensors, motion-activated energy-saving products, motion sensor switches, and Occupancy/Vacancy commercial solutions.
The Nuisance Factors: Blinks and Indicators
Modern energy codes, particularly strictly enforced ones like California’s Title 24, often mandate a “blink warning”—a visual signal that the lights are about to shut off. In a warehouse, this is a safety feature. In an oncology consult room, it is a psychological hazard.

I have walked sites where the system was programmed to flash the lights off and on five minutes before the timeout. Imagine a doctor delivering a difficult diagnosis—perhaps telling a patient that their cancer has returned. The room suddenly blinks. The patient, already in a state of high anxiety, often thinks the power is failing or an emergency alarm has been triggered. It shatters the moment. We must disable these warnings in patient care areas. Let the lights fade slowly if they must, or better yet, extend the timeout so it never happens during a consult.
There is a smaller, sharper annoyance that often goes unnoticed until the first patient complains: the sensor LED. Most motion sensors have a small LED (often green or red) that flashes every time it detects motion to prove it is working. If this sensor is mounted on the ceiling directly above the exam table, the patient is forced to stare at a flashing green strobe light while trying to explain their symptoms. It is hypnotic and irritating.
If you are doing a walkthrough, lie down on the table yourself—perform the “Gurney Test.” Look up. If a light is flashing in your eyes, put a piece of electrical tape over the sensor lens LED or program it off. The sensor still works; it just stops announcing its presence.
Code Compliance is not Clinical Competence
Expect pushback from energy auditors or LEED consultants who point to ASHRAE 90.1 or IECC tables requiring 15-minute timeouts and aggressive harvesting. They are reading the “Office” column of the code book.
You need to read the exceptions. Almost every major energy code, from IECC to local amendments in New York or Chicago, contains a clause for “Patient Safety” or “Clinical Necessity.” Section 9 of ASHRAE 90.1, for instance, often allows for exceptions where automatic shutoff would endanger patient care.
Use these exceptions. Document the clinical risk of a dark room. Specify a 30-minute or even 60-minute timeout for exam rooms. The energy load of three LED downlights running for an extra 15 minutes is a rounding error compared to the MRI machine down the hall. Do not let a strict interpretation of energy density compromise the primary function of the building, which is healthcare.
While we are discussing code, we must address dimming. Modern LED fixtures in healthcare are almost always 0-10V dimmable. However, keep the dimming control simple. A slide dimmer at the door is sufficient. Do not tie the exam room lights into a complex centralized building management system (BMS) that introduces lag. When a doctor hits the switch, the light must be there instantly.
The Golden Rule Spec
If you are writing the specification or approving the submittals for a medical office renovation, here is the non-negotiable baseline:
- Sensor Type: Dual-Technology (PIR + Ultrasonic) ceiling mount. No wall switch sensors (the view is too easily blocked).
- Location: Center of room, slightly offset to avoid direct glare for the patient, with a clear view of the physician’s workstation.
- Logic: Vacancy Mode (Manual-ON / Auto-OFF).
- Timeout: Minimum 30 minutes. Push for 60 if local code allows the exception.
- Nuisance: Disable all audible clicks, visible LEDs, and “blink warnings.”
The room should feel analog to the patient and the doctor. The technology should be invisible. If the doctor never thinks about the light switch, you have done your job.
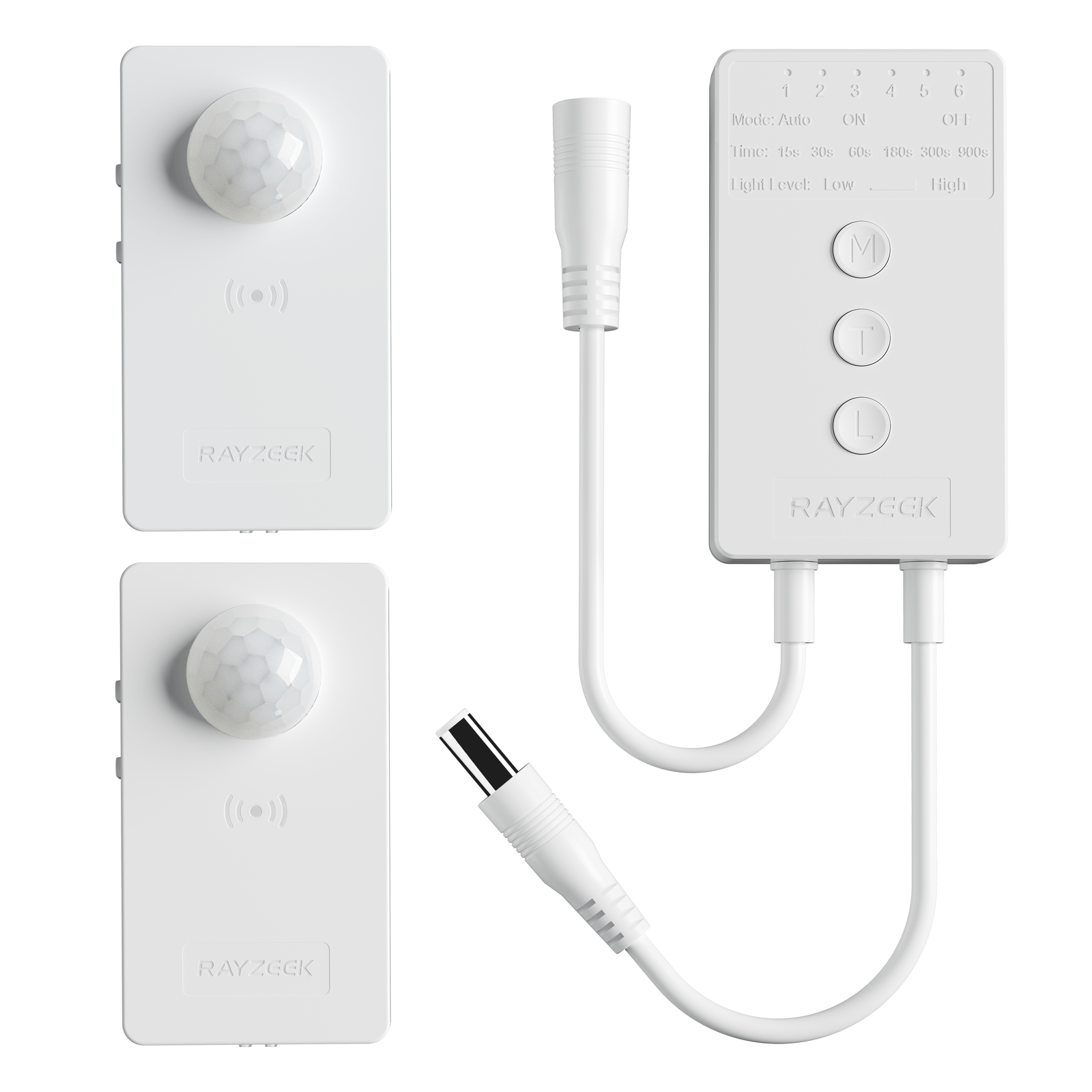
Get Inspired by Rayzeek Motion Sensor Portfolios.
Doesn't find what you want? Don't worry. There are always alternate ways to solve your problems. Maybe one of our portfolios can help.
Change Log
- Simplified the “immediate panic/immediate fury” sentence to be punchier.
- Rewrote the “managing kilowatt-hours vs. trust” line to break the repetitive rhetorical structure.
- Smoothed transitions in “The Physics of Invisibility” to sound less like a textbook definition.
- Changed “emotional container” to “shatters the moment” for more natural phrasing.