Medical spaces need intelligent lighting, but standard motion sensors often fail in clinics and exam rooms. A sensor that works perfectly in a hallway can create deeply uncomfortable moments in a space where patients undress or discuss sensitive health concerns. Imagine the sudden darkness mid-consultation, the awareness of being watched by an automated system during a vulnerable moment, or the distracting flicker of lights responding to small movements. Each of these moments erodes the trust that is essential to patient care.
The goal isn’t to avoid automation, but to implement it without sacrificing patient dignity. Motion-activated lighting offers real benefits: energy savings, hands-free operation for infection control, and consistent illumination without staff intervention. These advantages are compelling, but only if the system respects the unique demands of a clinical setting.
Exam rooms are not generic commercial environments. They require a different approach to sensor selection, placement, and configuration. When designed with an understanding of patient vulnerability and clinical workflow, motion control becomes an asset, not an intrusion. The principles for achieving this are grounded in the geometry of sensor coverage, the psychology of the patient experience, and the practical realities of medical practice.
Why Medical Spaces Demand a Different Approach
An office worker at a desk is not the same as a patient in an exam room. During a physical, a patient may be partially or fully undressed, positioned on an exam table, and focused entirely on the healthcare provider. This is not a transit space or a task-oriented environment. It is a room where privacy and comfort directly affect the quality of care.
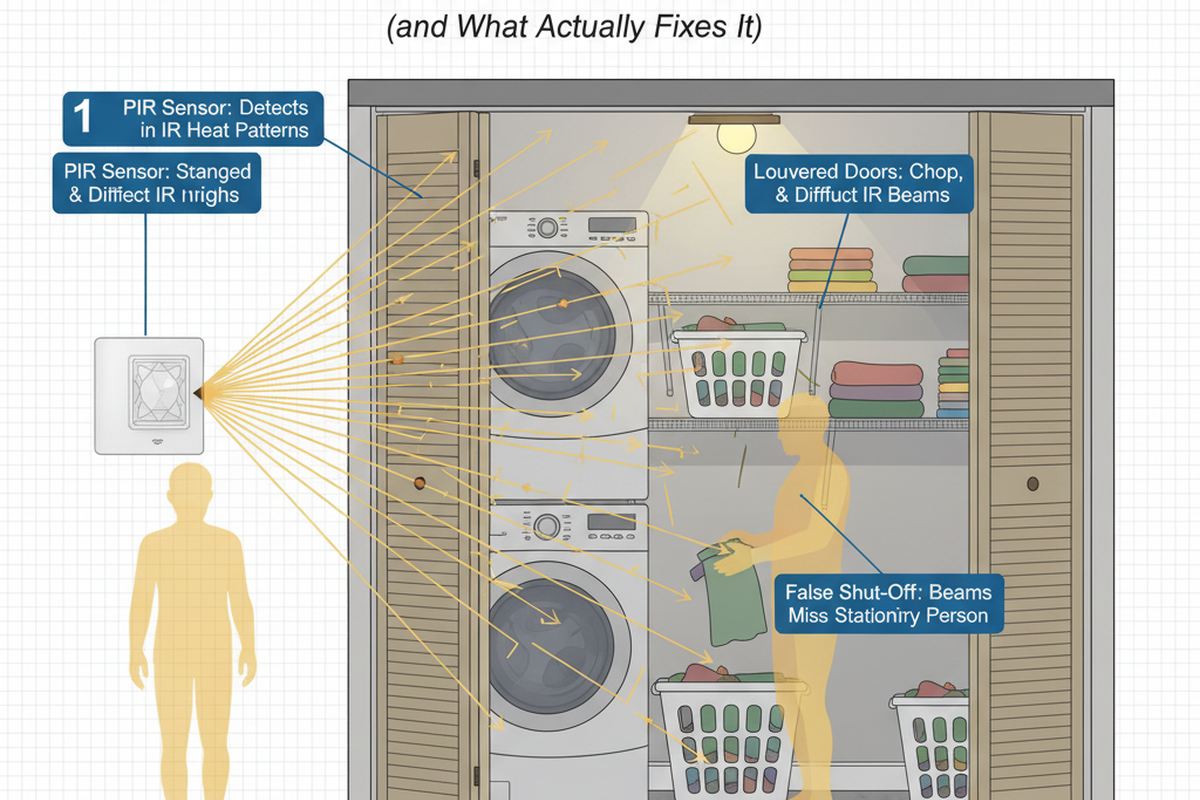
This vulnerability introduces a requirement that standard motion sensors are not designed to address. A sensor with a direct line of sight to the exam table does more than detect presence; it creates the psychological burden of being observed by a machine at a moment when the patient has already surrendered control. Even if a patient knows the sensor isn’t a camera, its presence is unsettling. The system installed to improve efficiency becomes a source of stress.
The nature of medical consultations presents another challenge. A follow-up may last five minutes, while a complex diagnostic discussion could extend to thirty. These conversations often include long pauses as a provider reviews records or a patient processes difficult news. During these moments of stillness, a sensor tuned for typical office activity will interpret the room as vacant and extinguish the lights. The disruption is jarring and unprofessional.
The trust a patient places in a medical facility extends to every element of the space. A light that behaves unpredictably or a timeout that feels arbitrary contributes to a sense that the room is not fully under control. In a setting where patients are already anxious about their health, the environment must feel reliable. Motion control that introduces uncertainty works against this core need. The room must feel designed for human care, not governed by inscrutable machine logic.
The Line-of-Sight Principle
The most critical decision in medical motion control is ensuring the sensor’s detection field does not have a direct line of sight to the patient during an examination. This isn’t about aesthetics; it’s about preventing patients from feeling watched by an automated system at their most vulnerable.
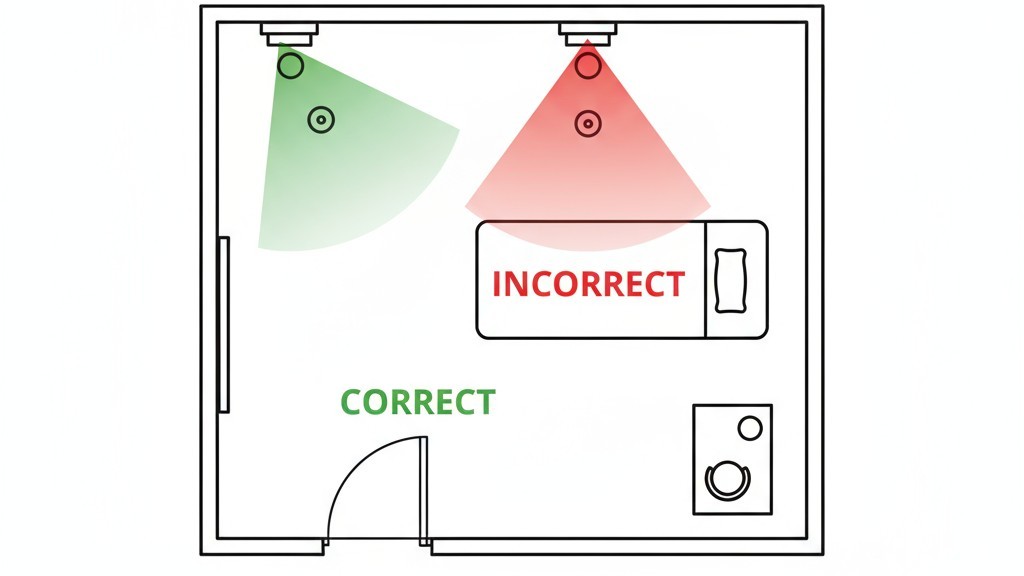
Passive infrared sensors work by monitoring changes in heat signatures within their field of view. This detection zone forms a cone extending from the sensor’s lens. If that cone is aimed directly at an exam table, it creates an implicit observation point. The solution is geometric: position the sensor to monitor entry points, circulation paths, and provider work areas, while deliberately avoiding direct coverage of the patient. The sensor can still detect occupancy reliably through indirect coverage, but it does so without creating the feeling of focused surveillance.
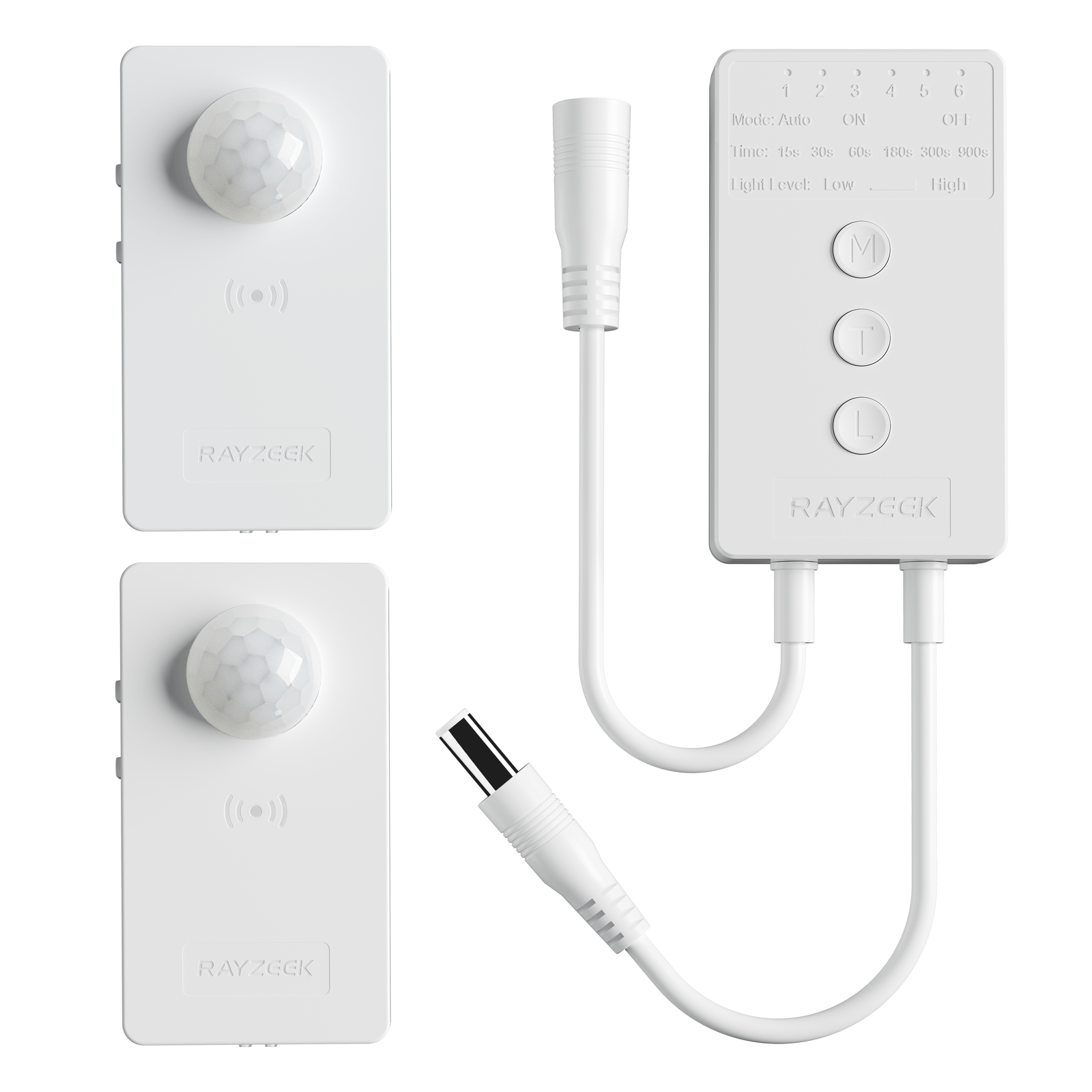
Get Inspired by Rayzeek Motion Sensor Portfolios.
Doesn't find what you want? Don't worry. There are always alternate ways to solve your problems. Maybe one of our portfolios can help.
Ceiling-Mounted Sensors: Coverage Without Exposure
Ceiling-mounted sensors are common in medical spaces for their wide coverage and unobtrusive profile. The key is to position the sensor closer to the room’s entry than to the exam table. A sensor installed near the door, or offset from the center of the room toward the entry, will capture movement as people enter and circulate without pointing its primary detection zone at the patient.
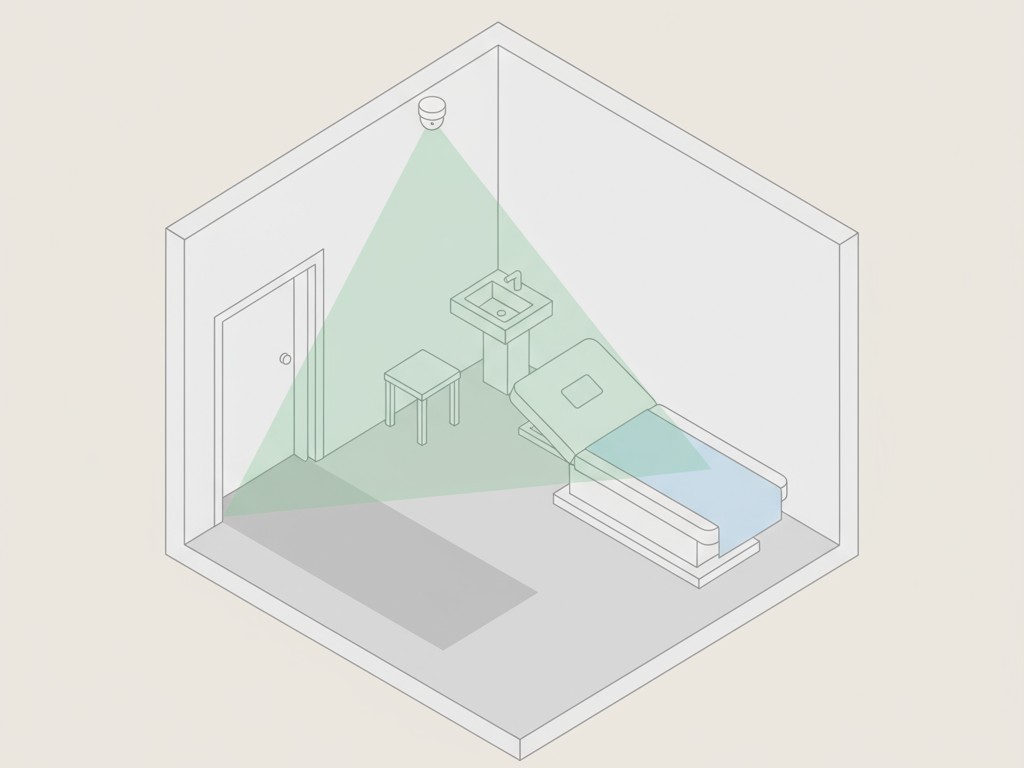
In a typical exam room, this means avoiding placement directly above the exam table. Instead, locate the sensor over the entry zone or the provider’s work area. Its detection pattern can then monitor the room’s active circulation while treating the exam table as peripheral to its field of view. The patient’s position should fall within the detection field’s edges, not at its focal point.
Wall-Mounted Alternatives
Wall-mounted sensors are a good alternative when ceiling placement is limited by fixtures or structural constraints. Their coverage is more restricted, so placement requires even greater care.

The best position is typically on the wall adjacent to the entry, aimed across the room’s width. This allows the sensor to detect entry and movement without pointing toward the exam table. A mounting height of seven to eight feet creates a horizontal sweep that monitors circulation rather than focusing on stationary positions. Wall mounting is often the best choice in rooms with drop ceilings, HVAC interference, or in retrofits where ceiling access is prohibitively expensive.
Occupancy vs. Vacancy Mode: A Critical Choice
The choice between occupancy and vacancy mode is fundamental. It determines who has control: the automation system or the room’s occupants.
In occupancy mode, the sensor is fully automated, turning lights on with motion and off after a timeout. This is ideal for hallways and storage rooms. In vacancy mode, a person must manually turn the lights on with a switch; the sensor only handles turning them off automatically after the space is empty. This preserves energy savings while giving control back to the user.
For an exam room, vacancy mode is superior. When a system automatically illuminates the room upon entry, it removes the patient’s ability to control their environment, compounding the sense of exposure. Vacancy mode restores a measure of agency. The patient or provider enters and makes a deliberate choice to turn on the lights, establishing a human decision point. The automation then operates quietly in the background, turning lights off only when the room is empty.
The recommendation is clear: specify vacancy mode for exam and consultation rooms. The trade-off is minimal—occupants simply flip a switch, a familiar action that requires no thought. In return, the system avoids the subtle discomfort of automated activation during a sensitive encounter. If budget constraints force the use of less expensive occupancy-mode sensors, then the other principles—careful placement and generous timeouts—become even more critical.
Timeouts That Build Trust
The timeout setting determines how long the sensor waits after detecting no motion before turning off the lights. In medical spaces, this is a primary factor in whether automation supports or disrupts the clinical workflow.
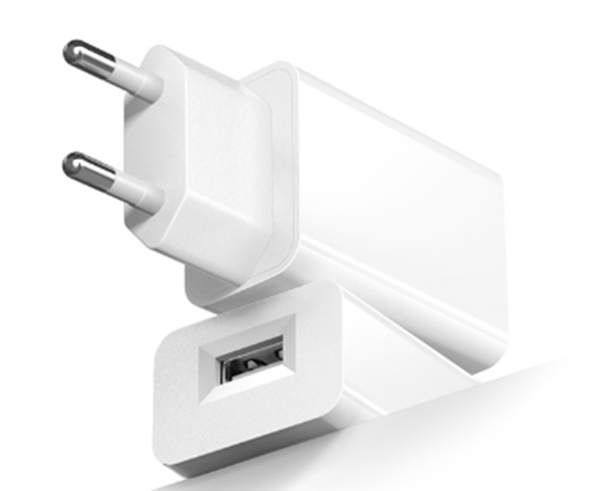
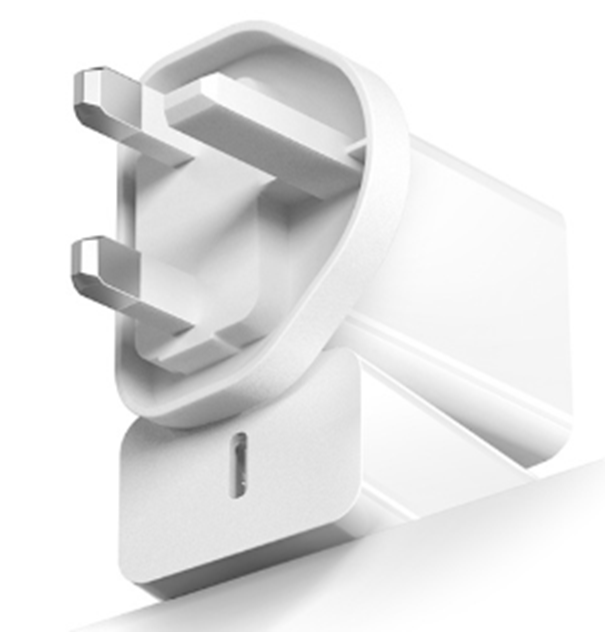
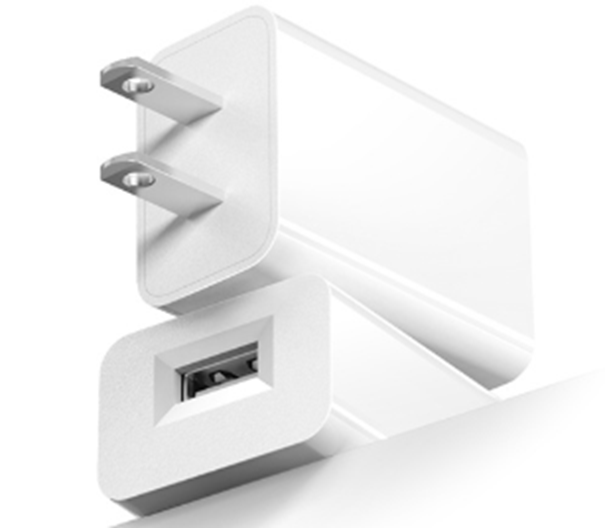
Looking For Motion-Activated Energy-Saving Solutions?
Contact us for complete PIR motion sensors, motion-activated energy-saving products, motion sensor switches, and Occupancy/Vacancy commercial solutions.
Consultations do not follow predictable motion patterns. A provider and patient sitting and talking may remain nearly motionless for extended periods. A standard five- or ten-minute timeout will trigger in the middle of such a conversation, plunging the room into darkness. The interruption is unprofessional and entirely avoidable.
Configure timeouts to accommodate the longest plausible consultation. A setting of 15 to 20 minutes provides a safe margin for most exam rooms. For spaces where complex case discussions are common, extending the timeout to 20 minutes or longer eliminates the risk of mid-session darkness. While longer timeouts slightly reduce energy savings, this is an acceptable trade-off. The goal is not maximum efficiency, but ensuring the automation never undermines the clinical encounter. A system that stays on for an extra ten minutes is far better than one that turns off during a serious conversation.
Rejecting Fidgety Behavior
Beyond settings, the physical behavior of the sensor system determines whether it integrates smoothly or becomes a distraction. Medical spaces demand motion control that is silent, steady, and invisible in its operation.
Noisy mechanical relays are a common problem. A loud click each time the sensor activates or deactivates announces the system’s presence. In a quiet exam room, this sharp mechanical sound is a disruptive intrusion, signaling that the automation is actively monitoring the space. The system should operate without an acoustic signature, using silent solid-state switching or dampened relays.
Hair-trigger sensitivity is equally damaging. A sensor that responds to the smallest movements—a patient shifting on the table, a provider reaching for a tool—makes the room feel unstable. Patients become hyperaware of the automation, conscious that their slightest gesture might provoke a reaction.
The system must be predictable. It should turn on when needed, stay on for the entire visit, and turn off only after the room has been empty for a defined period. It must do this silently and without distracting visual indicators.
Maybe You Are Interested In
The best motion control system is one that patients and providers never notice.
Adapting to Real-World Constraints
Ideal design conditions are not always available. Small rooms, multi-use spaces, and budget limitations require practical adaptations.
Small Exam Rooms
In a compact room, the ideal sensor placement may not be possible. A sensor near the door might still have a detection field that covers the exam table. In these constrained spaces, the goal is to minimize the directness of the line of sight. Mount the sensor as close to the door as possible to make the detection feel incidental rather than focal. Wall mounting on the entry wall, aimed horizontally, is often a better compromise than a ceiling-mounted unit in very small rooms. It may be necessary to accept reduced coverage in the far corners, but this is preferable to a sensor that creates an uncomfortable line of sight.
Multi-Use Spaces
Some rooms serve as both exam spaces and consultation offices, creating conflicting automation requirements. The exam function needs vacancy mode and long timeouts; the office function might be better served by occupancy mode and shorter timeouts.
When faced with this conflict, always configure the space for its most sensitive application: the exam room. A provider can easily tolerate manual light activation, but a patient cannot tolerate intrusive automation. The patient-facing function must take priority.